What is Sciatica?
Sciatica is a painful condition of the leg that may or may not be caused by back issues. Sciatica has many contributing factors and causes. This condition may be caused by spinal stenosis, facet referral, piriformis syndrome, or even a protruding or extruded disc. Sciatica is a term that is used loosely for pain going down the leg, however it doesn’t answer the question of, what is truly causing your my leg pain.
True sciatica should be felt in the entire lower leg as the sciatic nerve is responsible for all of the sensation in the lower leg. Feeling pains that radiate into the thigh and rarely going beyond the knee should be evaluated for other causes. Seeing a chiropractic orthopedist should be considered as a first stop to identify the true cause of the leg pain.
Is Leg Pain Sciatica?
No, not all leg pain is sciatica and in most cases leg pain is erroneously diagnosed as sciatica. The most common type of pain in the leg is sclerotogenous referral. Sclerotogenous referral happens when bone or tendons are the root cause of the pain such as joints and the insertion of a tendon into a bone. When a facet joint, or a back joint is injured, the brain is notified of the injury through a complex communication pathway. This pathway consists specifically of a small dorsal primary ramus nerve that constantly relays information to the brain about what position the joint is in (allows us to understand where our body is in space), and whether or not the joint has been injured.
If the joint is injured or even the ligaments that surround the joint, the facet capsules, the little nerve tells the brain in a pain signal. It also tells the postural muscles in that specific area of injury to lock down, this creates painful muscles the longer they stay splinted. This is why most people think its the muscle that is injured. This is not the case. It’s really a joint or ligament injury that causes a reflexive muscle splinting to help splint up the injured joint or ligament to allow for the joint to avoid further injury.
If we use the definition of sclerotogenous pain then we can understand why this type of injury termed facet syndrome, can create this type of pain. The muscles have become tighter to support the facet joints that are injured creating a tendinitis that can then refer pain into the buttock, hip, groin, outer thigh, top of the thigh, as well as into the knee. This is where the diagnosis of sciatica most commonly is given. In this condition the sciatic nerve is not involved and should not be diagnosed as sciatica, but more specifically should be diagnosed as referred sclerotogenous pain from facet syndrome.
A Chiropractic specialist in orthopedics in Fredericksburg can help with this type of referred pain by first, evaluating for the condition and diagnosing the problem. They can then decide whether manipulation is the right treatment for your condition. Other forms of treatment are available in Fredericksburg by a chiropractic orthopedist like, interferential TENS, ultrasound, flexion distraction, and others.
What Other Conditions Mimic Sciatica?
Once again we have to be careful using sciatica as a diagnosis because most times its not the sciatic nerve that is injured, rather another structure is injured that creates the leg pain. One of these structures while not as common as a facet joint injury, is one that most people fear, a bulging disc. This fear is almost always overplayed by the thought of having to get surgery. This is not true in a majority of these injuries and is only necessary when severe neurological deficits are seen. This includes bowel and bladder incontinence and saddle anesthesia (numbness on both inner thighs in the distribution of where we would sit on a saddle). This is a condition called cauda equina syndrome. While rarely happens is very severe and needs emergency decompression surgery.
Seeing a specialist is important while dealing with this type of leg pain and a chiropractic orthopedist should be a first choice. This is to ensure that these important signs and symptoms are constantly monitored while the initial conservative treatment is ongoing. These specialists are also able to get advanced imaging on the condition like MRI that tell the specialist how bad the disc problem is.
Most insurance companies will allow surgery after a certain period of time has gone by with conservative treatment. This is the most crucial time frame because this will be the deciding factor of whether surgery is performed or not. Most disc injuries will resolve on their own in 6 months, but during this 6 months it can certainly get worse as well. It is important to see a conservative management specialist like a chiropractic orthopedist in Fredericksburg, to make sure your condition continues on its way to proper healing without surgery.
This process starts with a very detailed evaluation testing for all nerve weaknesses as well as sensory changes, and most importantly arriving at the correct diagnosis. A chiropractic orthopedist in Fredericksburg will then utilize a treatment that is tailored to your diagnosis and may not include manipulation. At this point in time utilizing other forms of treatment like therapeutic epidural is not advised as this will block your bodies ability to tell you what positions and actions you need to avoid. This is really due to the epidurals powerful ability to block the pain that the disc problem creates.
Epidurals typically only last 6 months and if you receive one, it allows you to do a lot of the activities that are not helpful in your healing process and once it wears off you could have progressed into an extrusion, which may take an additional 6 months to heal. This leads most people to surgery wondering why the condition hasn’t gotten better or why it wont go away.
A bulging disc that has been diagnosed as a sciatica problem can be more harmful than helpful. A disc problem creating leg pain is more correctly termed radiculopathy while sciatica is termed more properly as a peripheral neuropathy as described below. Seeing a specialist in chiropractic orthopedics in Fredericksburg ensures the difference between the two are meticulously evaluated, and get you to resolution with sciatica treatment before the frustration of the condition leads to surgery.
Click here to read about protruding and extruded discs and how sciatica treatment in Fredericksburg can help.
Difference Between Radiculopathy and Peripheral Neuropathy (Sciatica)
There is a big difference between radiculopathy and peripheral neuropathy or sciatica. Sciatica is considered a peripheral neuropathy because the sciatic nerve is a peripheral nerve. For this conversation we will focus on peripheral nerves (sciatic nerve), and nerve roots. When a nerve root is injured it is a specific numbered nerve root ex. L1, L2, L3, L4, L5, S1 because it is the nerve root that comes out at that level of the spine. There are 2 nerve roots per level, a right and a left. Take a look at the diagram below for examples of nerve roots in the lower back as illustrated by Netters Atlas of Human Anatomy 6e.
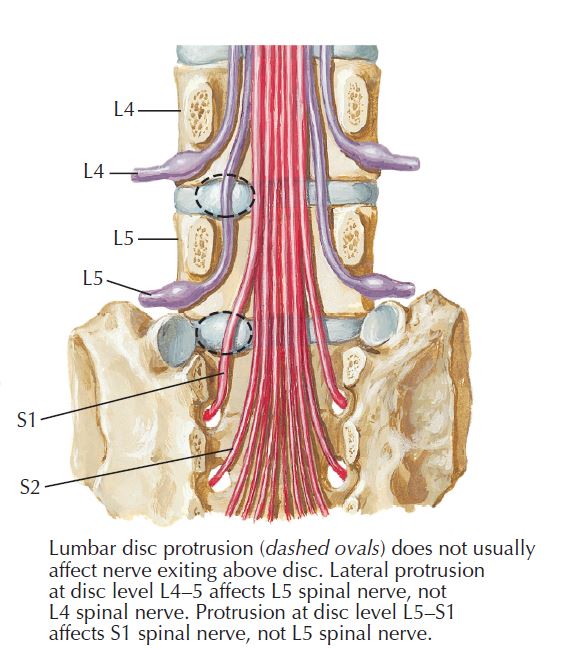
Each one of these nerves as they exit are termed nerve roots. when they continue outward and conjoin with different nerve roots they all combine to form what is termed a peripheral nerve.
The dotted line in the above diagram shows a disc protrusion could occur and what nerve root it would affect. The top dotted line illustrated what would be termed a L4/L5 disc protrusion affecting the L5 nerve root causing a left L5 radiculopathy. The lower dotted line illustrates a L5/S1 disc protrusion affecting the S1 nerve root causing left S1 radiculopathy. When a specific nerve root is affected it is more specifically called a radiculopathy and should not be called sciatica.
When a specific nerve root is affected it presents down into the extremity in a specific pattern called dermatomal. Look at the diagram below where these specific patterns are mapped out nicely by Dr. Netter from his Atlas of Human Anatomy 6e.
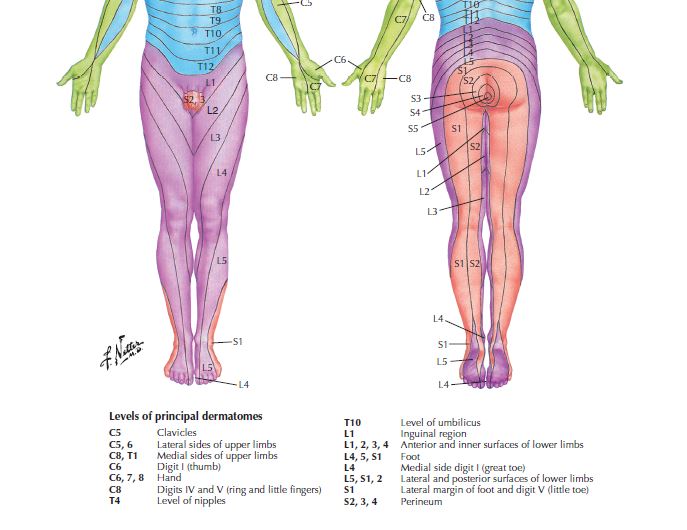
A lower body dermatomal map of referring pain into the specific distribution from an injured nerve root
If you look at the above diagram you will notice that a nerve root that is compressed will go down the leg in a specific pattern. For instance an issue affecting the L5 nerve root shows up as sensory changes to the outer thigh continuing into the outer calf and can get all the way down into the top and bottom of the foot. L4 comes all the way down the front of the thigh and continues into the inner calf and can go all the way down into the inside of the big toe. These are all examples of radiculopathy and a specialist like a chiropractic orthopedist uses this information to help determine the root cause of your symptoms.
Sciatica treatment, a peripheral neuropathy.
When talking about sciatica this is an example of peripheral neuropathy not a radiculopathy. The reason being this affects sensory areas that are not in a dermatomal pattern, rather they are in a pattern that multiple nerve roots combine to create the sensory area and not simply just one nerve root. Take a look at the diagram below, focusing on the area termed “sciatic nerve” and notice all of the nerve branches converging to form this large nerve. This is taken from Dr. Netter’s Atlas of Human Anatomy 6e.
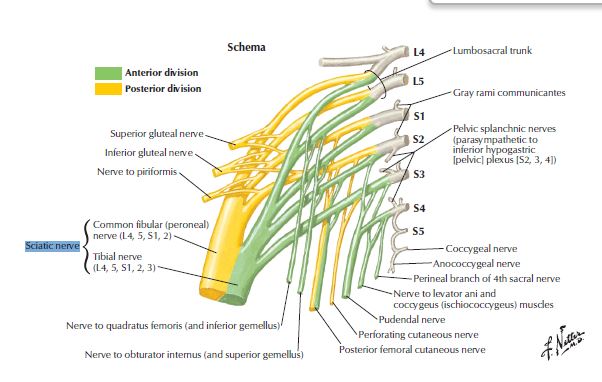
Illustration from Dr. Netter on the converging nerves to form the sciatic nerve. Sciatica treatment.
Because the sciatic nerve is formed from many different levels of nerve roots, L4, L5, S1, S2, S3, it will show up with sensory changes that do not follow a specific dermatomal map. Take a look at the below diagram focusing on the area highlighted as “from sciatic nerve”. This is the distribution that problems with the sciatic nerve creates sensory changes. Notice the picture does not show any sensory changes to the thigh or upper leg. Changes to the thigh or upper leg in this diagram are created by injury to a different peripheral nerve, the posterior femoral cutaneous nerve.
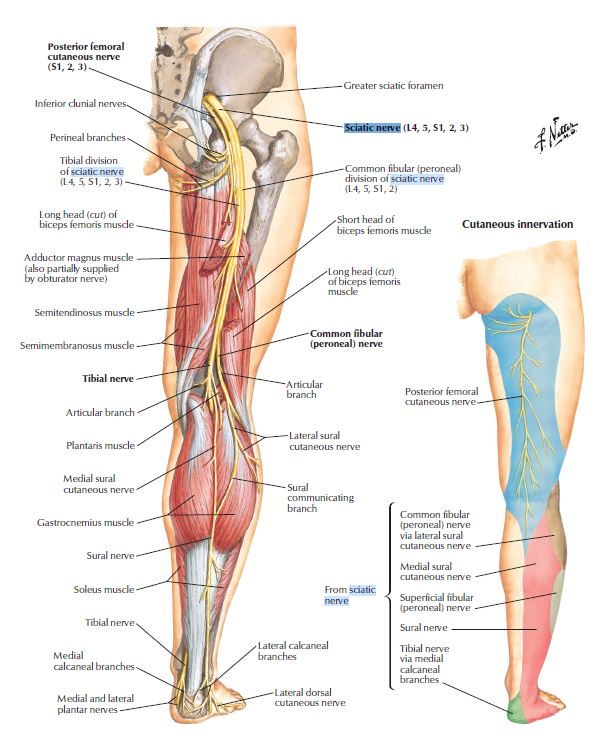
Pattern of sensory changes when the sciatic nerve is injured. Identifying the need for sciatica treatment.
What would cause Sciatic nerve compression?
One of the most common injuries to the sciatic nerve which rarely happens is due to compression via the piriformis muscle. This is a small muscle deep in the buttock that helps with external rotation of the hip. Its important to understand the sciatic nerves position in relation to the piriformis muscle which is in most cases below this muscle. In around 14-15% of the population this is not the case. In these individuals the piriformis muscle splits into two portions instead of one and the sciatic nerve exits through the two muscle bellies. This can create possible sciatic pains if the muscle becomes too tight and squeezes the sciatic nerve as it exits.
This condition is known as piriformis syndrome. Even though it has been documented as a known condition causing sciatic nerve irritation you should never assume this to be the problem without seeing a specialist who can arrive at your diagnosis. Take a look at the diagram below of Dr. Netters illustration of the sciatic nerve in relation to the piriformis muscle from his Atlas of Human Anatomy 6e.
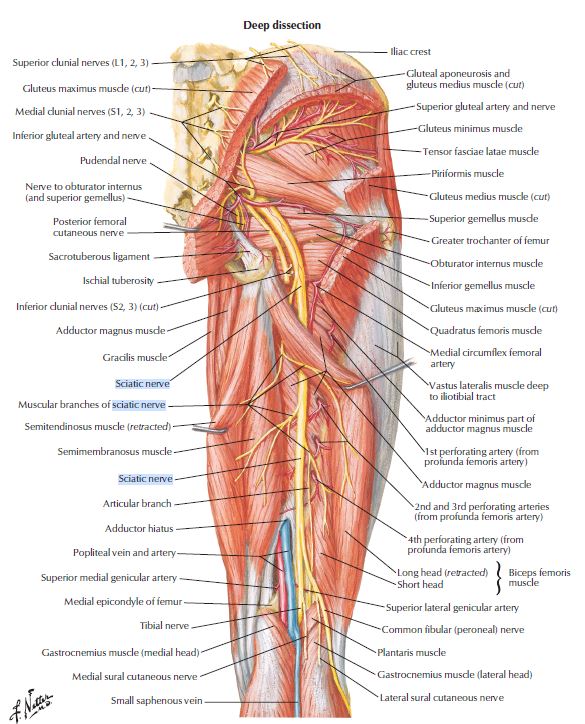
Picture illustrating the position of the sciatic nerve in relation to the piriformis muscle when thinking about sciatica treatment.
Is it Serious?
Sciatica is not necessarily always a serious condition, it depends on what is causing the sciatica. A chiropractic orthopedist sees these conditions on a daily basis and in most cases it is caused by facet referral into the thigh or leg. Other conditions commonly seen by a chiropractic orthopedist would be disc protrusion and extrusion. A protrusion or even an extrusion, can be more serious than the typical facet referred (sclerotogenous) pain, due to its volatility. When dealing with protrusion or extrusion it is imperative that you see a specialist that can quickly identify whether this is the case or not. This is because things like stretching or exercise may make these conditions worse especially if you are using them to try and self treat the condition.
Protruding discs if not properly diagnosed and treated can progress into a disc extrusion. This is what can happen if you perform stretches or heavy lifting. Look at the image below.
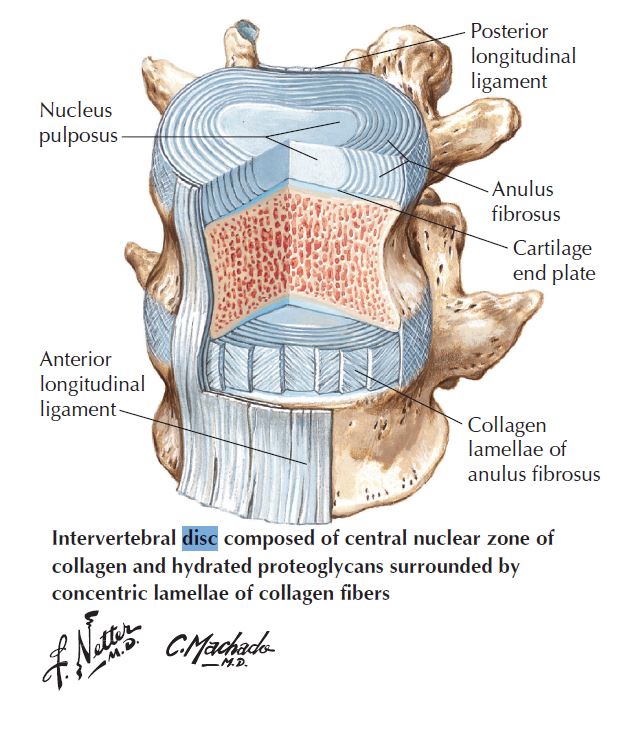
Disc as illustrated by Dr. Netter. Showing the nucleus and all the annular fibers. Sciatica treatment and causes.
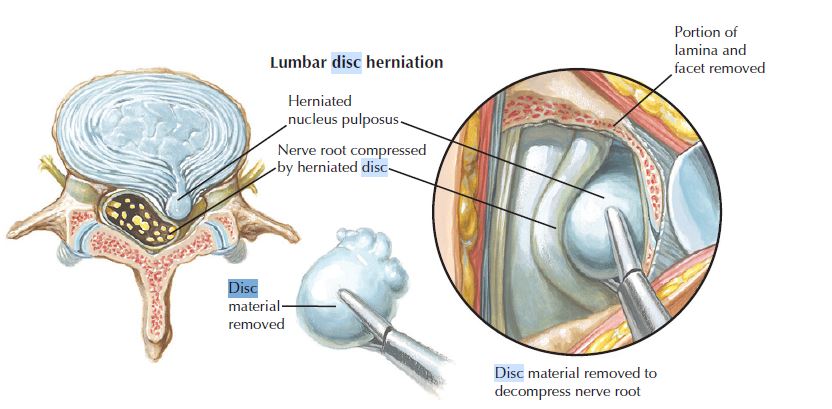
Lumbar disc herniation as illustrated by Dr. Netter. In this case the nucleus has gone through all the layers of the annulus and can be termed more correctly as extrusion as used in our writing.
What we see in a disc is a center of jelly surrounded by fibrous rubber band like rings that contain the center core. The disc takes 85% of the compression in the spine and does well with the stress until the little rings start to tear. Tearing of the fibrous rings doesn’t necessarily create any pain, at least not until enough of those fibers tear to allow tearing to continue into the outer 1/3 of the collection of rings. When tears occur in the outer third this creates a lot of pain, normally felt as back pain with or without leg pain. When the rings tear it affects the integrity of the disc by allowing the jelly to start moving outward creating a bulge or protrusion. If the bulge is big enough it will contact one of your spinal nerves and give you very sharp almost electric like pain down into a specific section of the leg.
This is more correctly termed radiculopathy (the pain down into the leg). When radiculopathy is the cause of sciatica then the condition needs a specialists attention, a specialist like a chiropractic orthopedist will be able to diagnose and treat the condition conservatively without the use of surgery in almost all cases. When a protrusion gets worse from daily activity and proper diagnosis has not yet been performed, the protrusion can progress to an extrusion. This condition is worse in only the sense that the jelly now has broken through all fibrous rings and is now considered uncontained. This condition typically does not get worse, in fact the low back pain may resolve making the leg pain the main complaint and is continuous regardless of position. It is at this point as it has no more fibrous rings to tear and progression of the condition only happens due to the inflammatory response needed for proper healing. As inflammation sets in the inflammation is very close to sensitive nerves that deal with sensation as well as motor. This means muscle weakness can start to happen if it hasn’t already from the protrusion.
It is important to see a specialist like a chiropractic orthopedist to determine whether this is the cause of your sciatica right away. The chiropractic orthopedist is also able to do certain tests that tell them how severe it is like muscle testing and sensory testing. They will then monitor you throughout the treatment plan to make sure that symptoms are getting better and not continuing to get worse. Chiropractic orthopedic specialists, while they are licensed to perform manipulations or adjustments, may elect different treatments in the initial stages. Some of these treatments are TENS, ultrasound, manual traction, and simple education of the condition you have and on ways to take care of it at home to make sure healing is expedient.
Sciatica Treatment, Stretches in Fredericksburg
Stretching for sciatica should never be done until proper diagnosis has been reached. Your treatment for sciatica needs to be specific to make sure that we are not injuring the condition. Stretches may work for the sciatica pain but it will also stretch the deeper tissues that if they are the root of your pain, shouldn’t be stretched. If the stretching you’ve done helped the back pain but the leg still continues to hurt and may even be worse, you have created another issue. Always seek the help of a board certified specialist when dealing with sciatica. Do not stretch through the pain, get evaluated.
Will it go away on its own without sciatica treatment?
In most cases it will go away on its own, however not if you are uncertain of how to deal with sciatica. Depending on diagnosis once again certain things can make certain diagnoses worse. The best chance to see if your sciatica goes away on its own is to listen to your pain, don’t try to mask it. Masking it allows for us to do everything before the sciatica began but this may not be best for the condition. Pain is the way the body tells us that a certain position, posture, or task is injuring the damaged tissue. Listen to it. Finding a position that makes the pain go away or lessens the pain to its least severity is best. Some of these positions can be found in the article of spine sparing strategies in Spotsylvania.
When Considering Sciatica Treatment, Could it be a Problem With the Hip or Bursa?
Sciatica is not likely caused by a hip out of place or a bursa inflamed. Generally hips that are out of place only happen in childhood and are called hip dysplasia. This is a condition for an orthopedic surgeon to fix. Hips that are out of place need surgery and do not happen often unless trauma is involved. Hips also do not get aligned by chiropractic manipulation or get “put back in”. Manipulation is used to aid in damaged joints that may contribute to hip pain or sciatica. The hip is not being repositioned during a manipulation, the joint as well as the ligaments that support the hip make this nearly impossible.
Seeing a chiropractic orthopedist will ensure proper imaging is done to rule out the hip as a possible sciatica pain source. If the chiropractic orthopedist determines on x-ray that the hip joint is degenerated they may decide to start a trial of conservative treatment to figure out how much of the pain is related to the back and how much is in the hip. If the chiropractic orthopedist determines the majority of pain is from the hip alone then they may send you for a surgical consult.
The bursa that are in the hip may become inflamed when we have problems to the muscle tendons in the area. The idea here is that the tendon is the problem not the bursa. Bursa are small fluid filled sacs that allow for the tendon to slide easier when we use the muscle. Bursa are filled with synovial fluid and produce more when they are inflamed or being overused by the damaged tendon. The focus here should be on working with the tendon and allow the bursa to calm down and return to normal when the source of the problem is properly treated.
When you have sciatica, one of the sciatica treatments that you may be offered is an injection. These injections come in many forms. Trigger point injections, steroid injections into a joint, epidural injection, injections into the bursa, all of these aim to remove the pain that is being felt. This can be a double edged sword in that if it works, great. If it doesn’t then the quest for diagnosis continues. It may have changed your pain a little bit, probably made the pain a little better, but depending on the injection may make the diagnosis harder to achieve. Some of these injections if they contain a steroid, will help with inflammation and also the pain that you feel. This can be detrimental during physical exam when you are not responding to the test that they are performing to diagnose the condition. Steroid injections also alter the blood flow to the area, and while pain gets better, will prolong the overall recovery period. Inflammation is not always bad. The body needs inflammation to heal and if we stop the bodies process of healing, healing is becomes longer.
There are specific situations when the sciatica treatment of a steroid injection should be avoided. These include before diagnosis has been met, and anytime that it is being used for suspected disc protrusion. This comes in the form of therapeutic epidural. If you are trying to avoid surgery then a therapeutic epidural should be reserved for extrusion only not a protrusion. A protrusion is considered a contained disc and may be the cause of your sciatica. If an epidural steroid injection is given at this time, pain will subside. This may feel nice but it increases your risk of extrusion. If you get the epidural steroid injection and the pain gets better because your blocking the pain signals, how is the body going to tell you that you are doing too much and are risking injuring it further? It can’t. This could be a more harmful type of sciatica treatment.
In these cases we see a situation where the pain goes away for 5-6 months but then comes right back. This makes the sciatica sufferer seek more answers and sciatica treatment, which usually lands them in the surgeons office. Now that the 6 weeks of conservative care has been met surgery is on the table now. This is because the 6 months of pain relief has allowed the individual to continue everything as normal and shouldn’t have. The disc now extrudes and presents itself as sciatica pain all over again after the epidural steroid injection wears off. This may be a little different now, and could possibly be only leg pain without the previous back and leg pain.
It’s always best to start with conservative measures before any other form of sciatica treatment, especially if you are trying to avoid surgery. Seeing a chiropractic orthopedist for sciatica treatment can be beneficial for correctly diagnosing the condition, educating about the condition, and treating it without the use of surgery or invasive steroid injections that can alter the bodies normal responses.
If you are in need of a sciatica treatment specialist in Spotsylvania or Fredericksburg to manage sciatica issues, don’t hesitate to contact us at Stine Chiropractic Clinic. With the areas only board certified chiropractic orthopedists, we are equipped to get you the diagnosis and treatment you need for any of your orthopedic concerns. See us for sciatica treatment today!