What really is a pinched nerve? Most people will have heard it sometime in thier life. In a general sense It’s exactly what it sounds like. Something is causing compression to a nerve and creating painful symptoms. But the real question is, what. What structure of structures have the potenttial to compress nerves? If you answer this question than proper treatment can be rendered. This is the aim of a chiropractic orthopedist, to evaluate and diagnose, what is truely “pinching the nerve.” Spinal stenosis, foraminal stenosis or a soft tissue injury is capable or pinching a nerve.
What structures can cause a “pinched nerve.”
When evaluating the different structures that can lead to pinched nerve, there are a few categories that it may fall under. Soft tissue, and hard or bony tissue. Soft tissue causes include muscle, and disc injury that can compromise the space the nerve needs to travel without being “pinched.” Bony or hard tissue causes are typically from bone, like the vertebrae and their components. Bony causes typically have some sort of degenerative process involved or age related changes. They can also be things present at birth, or congenital.
Soft tissue causes
Repetitive and overuse injuries have the ability to change the size of the muscle. Nerves travel down the spinal column and exit at a certain level. After they exit they continue to travel through the body to their effector muscle or sensory receptor. When traveling to these sites, any change in size of the surrounding muscles in the nerves route, can cause impingement or “pinching.” A good example of this is carpal tunnel syndrome. Carpal tunnel syndrome occurs when the tight band that supports the wrist compresses the inner contents. One of these contents is the median nerve which is responsible for the sensation to the thumb, index, middle and thumb side of the ring finger.
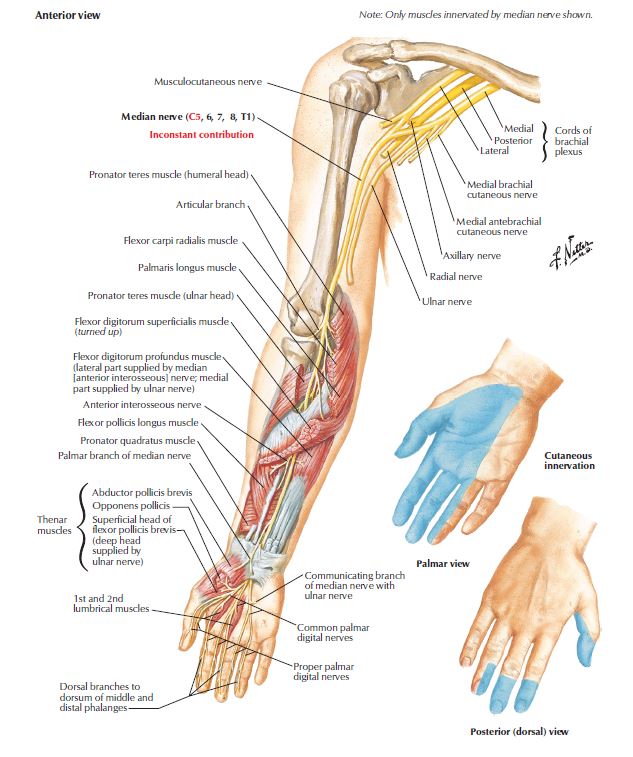
The median nerve supplies the thumb, index, middle and the thumb side (half) of the palm. Comprssion of this nerve creates sensory changes in the area here depicted in blue. Illustration by Frank Netter Atlas of Human Anatomy 6th edition.
Protruding disc causing “pinched nerve”
The most common type of soft tissue creating “pinched nerve,” is from the discs in the spine. These are the load bearing structures of the spine and are subject to injury. When discs become injured, the little firbrous bands that keep the center jelly contained tear, and this allows for migration of the jelly. This can create an outward protrusion of the disc that can compress the nerves at the back side of the vertebrae.
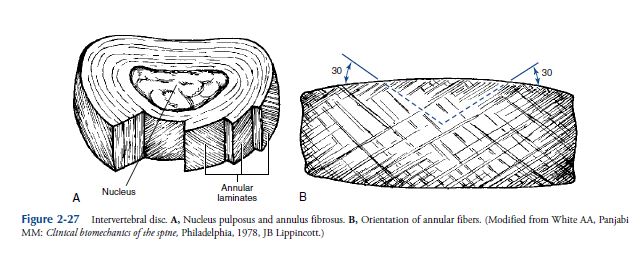
Normal anatomy of the intervertebral disc. With a central gelatinous core and an outer fibrous perimeter made of about 23 layers or elastic bands alternating in fiber orientation to increase tensile strength.
When a disc begins to protrude it can contact an exiting nerve root or “pinch” a nerve root sending pain in that levels dematomal pattern. L4/SL5 disc protrusion affects L5 nerve root, sending L5 dermatomal pain pattern. Likewise L5/S1 disc protrusion “pinches” the S1 nerve root, sending S1 dermatomal pain pattern.
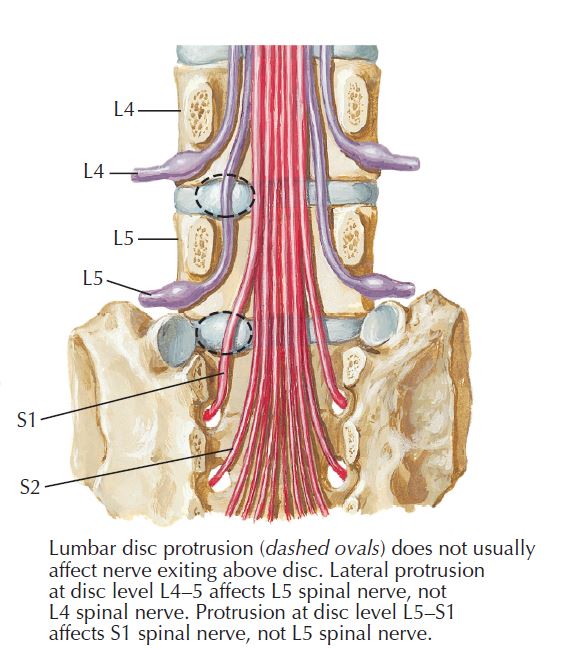
Compression of a nerve root due to bulging or protruding disc. Each of these spinal nerves, when compressed or pinched by the disc, will correspond to its dermatomal level.
When this happens severe extremity pain can be felt. This travels down a specific sensory distribution that corresponds to the disc level involved. This type of pain is called dermatomal.
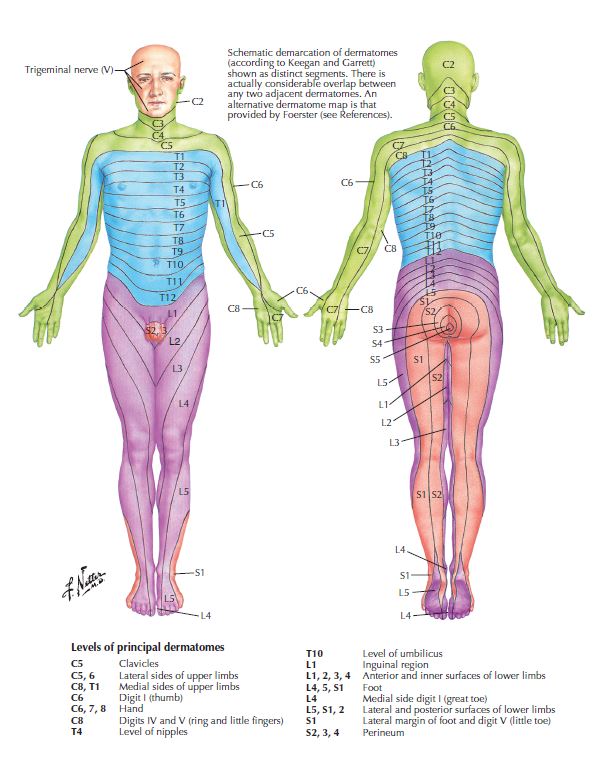
This is a dermatomal map of the different patterns an individual may experience feeling changes when the specific nerve root is injured or compressed. Illustration by Frank Netter Atlas of Human Anatomy 6th edition.
Bony or degenerative changes causing “pinched nerve”.
Foraminal and spinal stenosis. These are two separate conditions, that may be present at the same time. Spinal stenosis is a narrowing of the vertebral foramen, while foraminal stenosis is narrawing of the intervertebral foramen.
Spinal stenosis (vertebral foramen stenosis).
The symptoms of spinal stenosis can vary from mild to severe depending on the amount of stenosis and at which level in the spine it is present. For instance the spinal cord travels through the foramen magnum (hole in the base of the skull) and all the way down to the first or second lumbar vertebrae. After this point it continues as the cauda equina which is just a cluster of spinal nerves. Injury to the spinal cord in almost all cases is severe and permanent however injury to spinal nerves may not be. The cord and brain are considered the central nervous system, and injury here creates severe and permanent disability. Spinal nerves are considered a part of the peripheral nervous system, damage here at this level can be permanent, but most of the time is only transient. This is due to the fact that peripheral nerves regenerate. Central nerves do not regenerate and this is why the difference in severity and pemanency of damage or injury to the different types of nervous system matters.
With the above being said, the cervical and thoracic vertebral foramen contain spinal cord. Spinal stenosis at these levels can have severe consequences. The lumbar spine vertebral foramen contain spinal nerves. Stenosis at this level has varying degrees of severity. Spinal stenosis in most cases is present from birth and may become a problem later on in life if combined with other conditions like our next topic, foraminal stenosis.
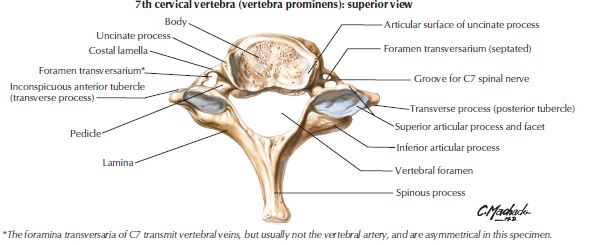
Depiction of superior view of the cervical vertebra showing the vertebral foramen. illustrated by Macado, Atlas of Human Anatomy 6th edition.
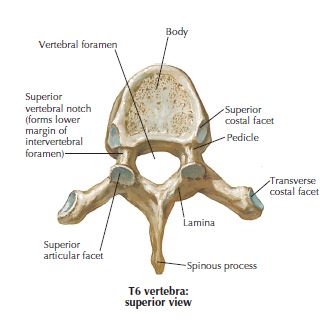
Superior view of the thoracic vertebra showing the vertebral foramen.
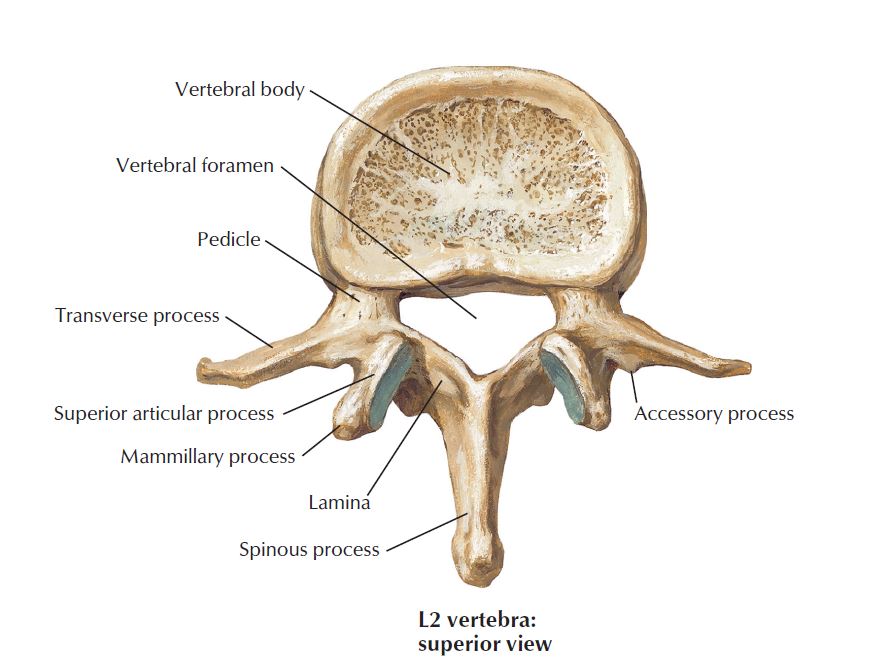
Vertebral foramen of the lumbar spine. Illustration by Frank Netter Atlas of Anatomy 6th edition.
Foraminal stenosis (intervertebral foramen stenosis) “pinched nerve”
This is the most common form of stenosis leading to a pinched nerve of bony origin. Coupled with spinal stenosis the symptoms experienced can be quite severe and chronic. Foraminal stenosis is narrowing of the intervertebral foramen, the hole that exists between two adjacent vertebrae. All intervertebral foramen have an exiting nerve root that can be “pinched” if narrow enough. A spinal nerve being a peripheral nerve, means these symptoms, in some cases can be reversed. This is due to the spinal nerves ability to regenerate.
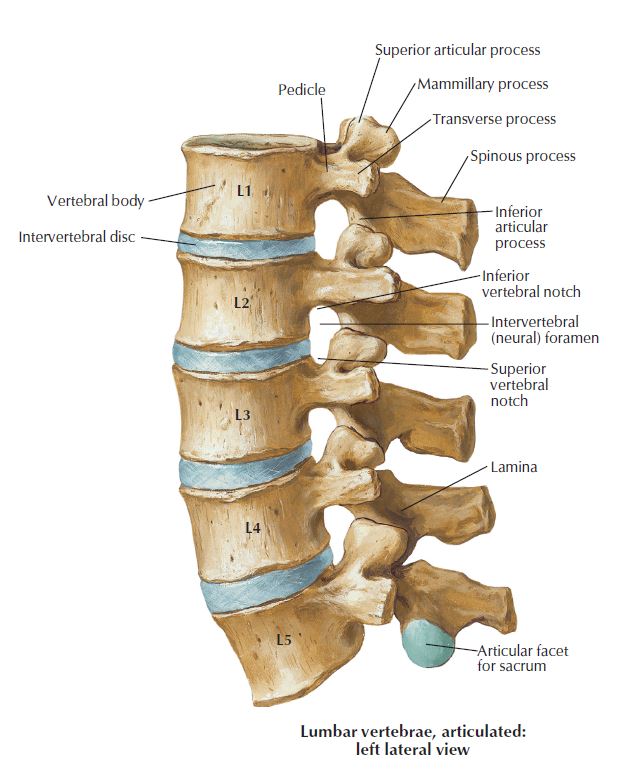
Intervertebral foramen or neural foramen. This contains the exiting nerve root. Pinched nerve here causes radicular or dermatomal patterned pain this is foraminal stenosis. Lumbar spine.
Foraminal stenosis symptoms can mimic a disc lesion. This is due to its pain distribution pattern. Much like a bulging disc the “pinched” spinal nerve has a specific pattern that it travels into the extremity that gives the clinician an objective insight into which foramen is involved. This happens in a dermatomal distribution.
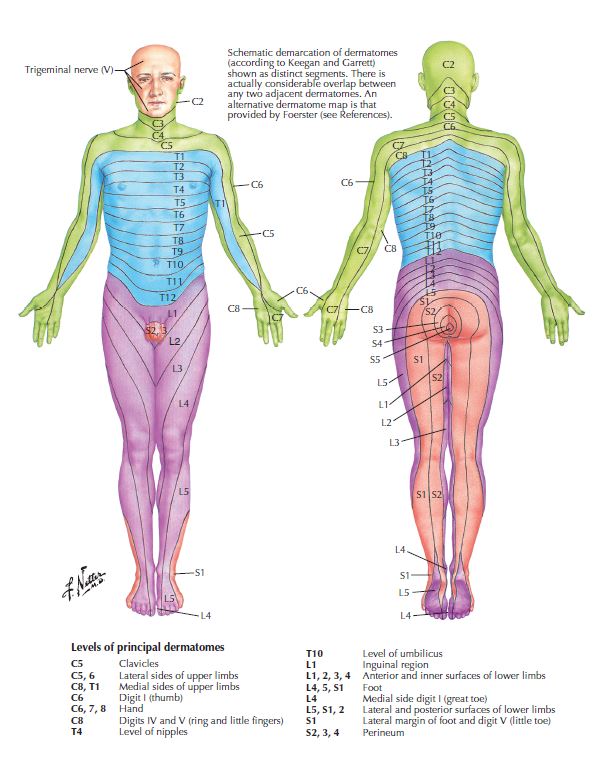
This is a dermatomal map of the different patterns an individual may experience feeling changes when the specific nerve root is injured or compressed with foraminal stenosis.
Is surgery necessary for spinal stenosis?
Most cases no. If you have very severe spinal stenosis in the cervical or thoracic areas with severe symptoms like involuntary jerking motions and trouble with walking called ataxia, then surgery should be considered. If these symptoms are present then you need to be seen by a surgeon urgently. Only a few cases of spinal stenosis are this severe, and surgery should only be considered if all conservative measures have been tried with no relief. Seeing a chiropractic orthopedist is a good place to start if you have spinal stenosis. These specialists can monitor the condition for any conserning worsening.
Is surgery necessary for foraminal stenosis?
No. The only time that surgery is necessary is if all conservative measures have failed and the individual patient wishes to try surgery as an intervention.
Is surgery necessary for a bulging disc?
No, unless you have the severe symptoms of uncontrolled movements and trouble walking called ataxia. This can happen in the cervical and thoracic areas as the disc can compress spinal cord and not just spinal nerves. We have very strong ligaments behind the vertebral bodies that keep a disc from bulging directly into the spinal cord. A bulging disc is more likely to bulge posterolaterally, or the posterior and lateral portions of the spinal foramen.
The lumbar spine does not have as much of these ligaments that the cervical and lumbar do, as it tapers the farther down in the spine we go. The lumbar spine only needs surgery when symptoms like bowel and bladder incontinence, and numbness in the saddle area are experienced. This could be cauda equina syndrome and may need emergency decompression surgery. This condition once again is very rare.
Benefits of seeing chiropractic orthopedist for conservative treatment.
Seeing a specialist like a chiropractic orthopedist can help through proper diagnosis of the condition you are suffering with. Diagnosing the condition and correlating the clinical symptoms and their severity can help determine whether surgery is actually necessary. There are many different tests that a chiropractic orthopedist can use to aid in proper diagnosing like physical exam, MRI, X-rays, and neurological testing.
When is the best time to see a chiropractic orthopedist for a “pinched nerve.”
Seeing a chiropractic orthopedist when your symptoms are active is always a good idea. When spinal or foraminal stenosis has been a diagnosis in the past, sometimes this may not be the direct cause of current complaints. Seeing a chiropractic orthopedist can help you get the answers about whether or not the stenosis is the cause or just a complication that leads to episodes of another common condition that is responsive to treatment.
Read more on specific conditions.
- Disc protrusion.
- Disc extrusion.
- Spinal stenosis.
- Foraminal stenosis
- Peripheral neuropathies like: Carpal tunnel, cubital tunnel, sciatica, thoracic outlet.